Behavioral health billing &
revenue cycle management in one system
Connect eligibility, authorizations, encounters, claims, ERAs, and client payments into one clean workflow. So you get paid faster with less rework.

A single system for clinical care and behavioral health billing
Ritten automatically generates the right claims for inpatient/residential billing whether you bill by encounter, bundle encounters into per diem, or generate per diem claims from program enrollment. We offer flexible ailling automation that matches how programs actually bill.
For Clinicians
For Billers
For leadership & owners
How Ritten supports your behavioral health revenue cycle
Ritten connects every step of your RCM process. Data is collected once, then flows through authorizations, claims, ERAs, and reporting automatically; eliminating the gaps that cause denials, delays, and administrative burden.






Revenue cycle management designed for behavioral health realities
Ritten isn't a generic medical billing add-on. It's designed for the operational and regulatory complexity of behavioral health; group therapy, stepped levels of care (OP → IOP → PHP → residential), Medicaid requirements, and multi-location workflows.
.png)




Billing tools that respect clinical work and compliance
Ritten keeps a clear line between what happens in the chart and how it's billed. Clinical teams document care; billing teams configure rules and claims. Authorizations, diagnoses, and services stay aligned so you can:




From Billing Chaos to One-Hour Workdays
Megan, a billing leader at a behavioral health clinic, used to spend hours jumping between EMRs, billing software, and payer portals to resolve claims and reconcile payments.
After switching to Ritten:



Now, she completes her daily billing work in about an hour; without wrestling multiple systems all day.


Frequently Asked Questions
Still have questions about ourbehavioral health software? Email us at info@ritten.io
Yes. You can set up workflows to automatically charge client copays once claims are processed and payer responsibility is clear.
Ritten supports electronic claim workflows commonly used in healthcare revenue cycle operations, including preparing claim data for submission and reconciling remittance information. Exact connectivity (clearinghouse, payer connections, ERA, and status transactions) depends on your configuration and integration requirements.
Yes. Behavioral health organizations often bill using a mix of per diem (residential/inpatient), bundled case rates, and fee-for-service (outpatient, professional services). Ritten can be configured to support common billing structures and payer-specific rules, including authorization-related constraints.
Many organizations use a clearinghouse or billing partner. Depending on your model, Ritten can support that workflow through integrations, exports, or APIs. We’ll confirm your clearinghouse and billing setup during scoping.
Authorizations are linked to payers and CPT codes. When you bill, Ritten applies the appropriate auth details to the claim automatically.
Payments are linked to specific services and claims, so your A/R and client balances stay accurate and audit-ready.
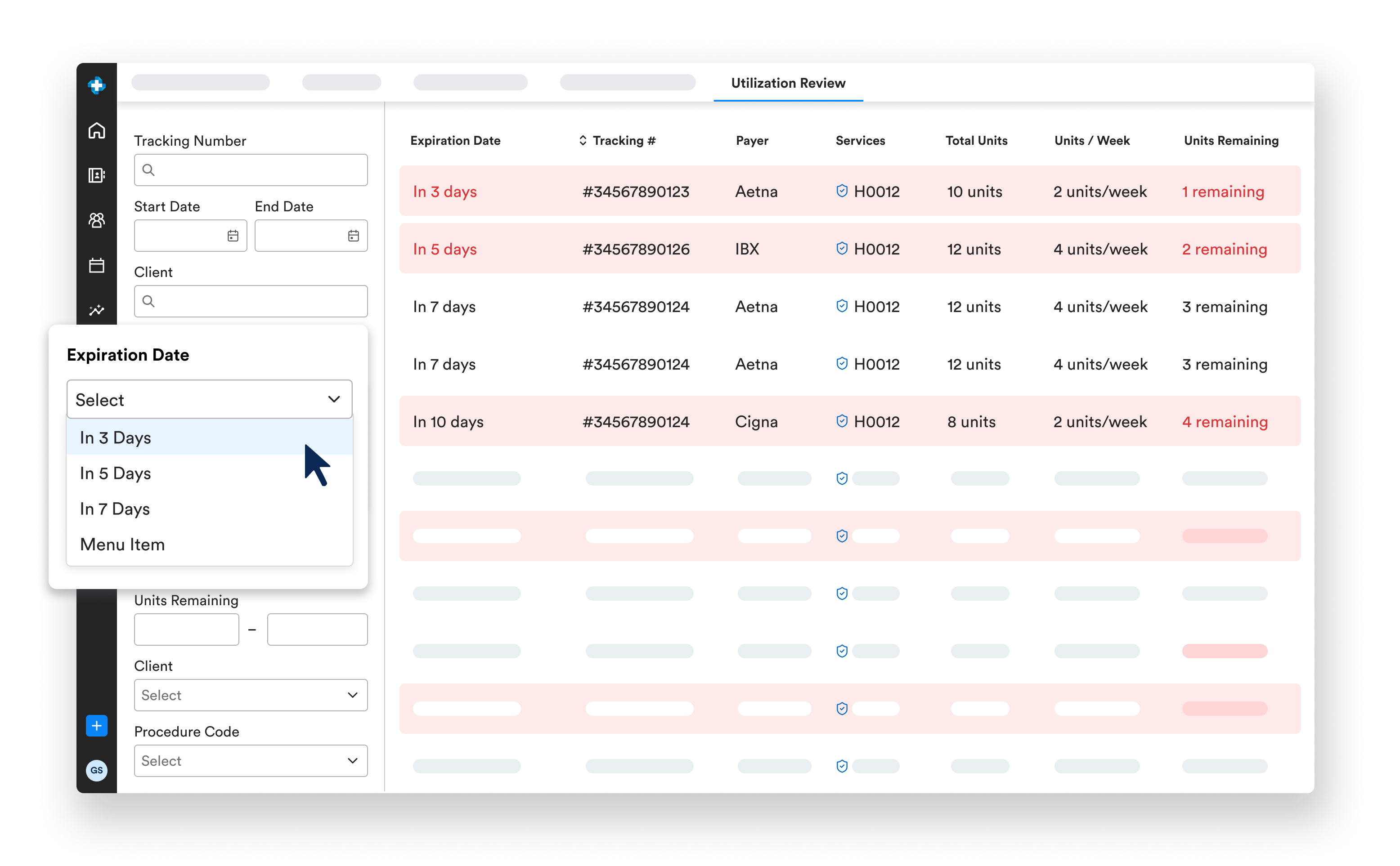
Ritten supports capturing authorization and payer requirements and can connect encounter and documentation workflows to authorization rules. This is especially important in higher levels of care where approved dates, units, and medical necessity documentation must align to avoid denials.
Ritten is designed to connect documentation to billing requirements. Organizations can configure billing rules and documentation checks so missing required fields, unsigned notes, or incomplete encounters are identified early. Clean-claim workflows reduce rework, denials, and delays in reimbursement.
Ritten RCM is the revenue cycle component of the Ritten behavioral health platform. It connects clinical encounters and documentation to billing workflows to help programs generate clean claims, manage payer requirements, track authorizations, and improve cash flow through better visibility into the billing pipeline.
Ritten supports configurable reporting that can include billed vs. unbilled volume, aging and A/R indicators, payer mix, denial categories, and operational throughput metrics. The specific dashboards and exports depend on your payer contracts, encounter structures, and finance reporting needs.

