Behavioral health authorizations under control
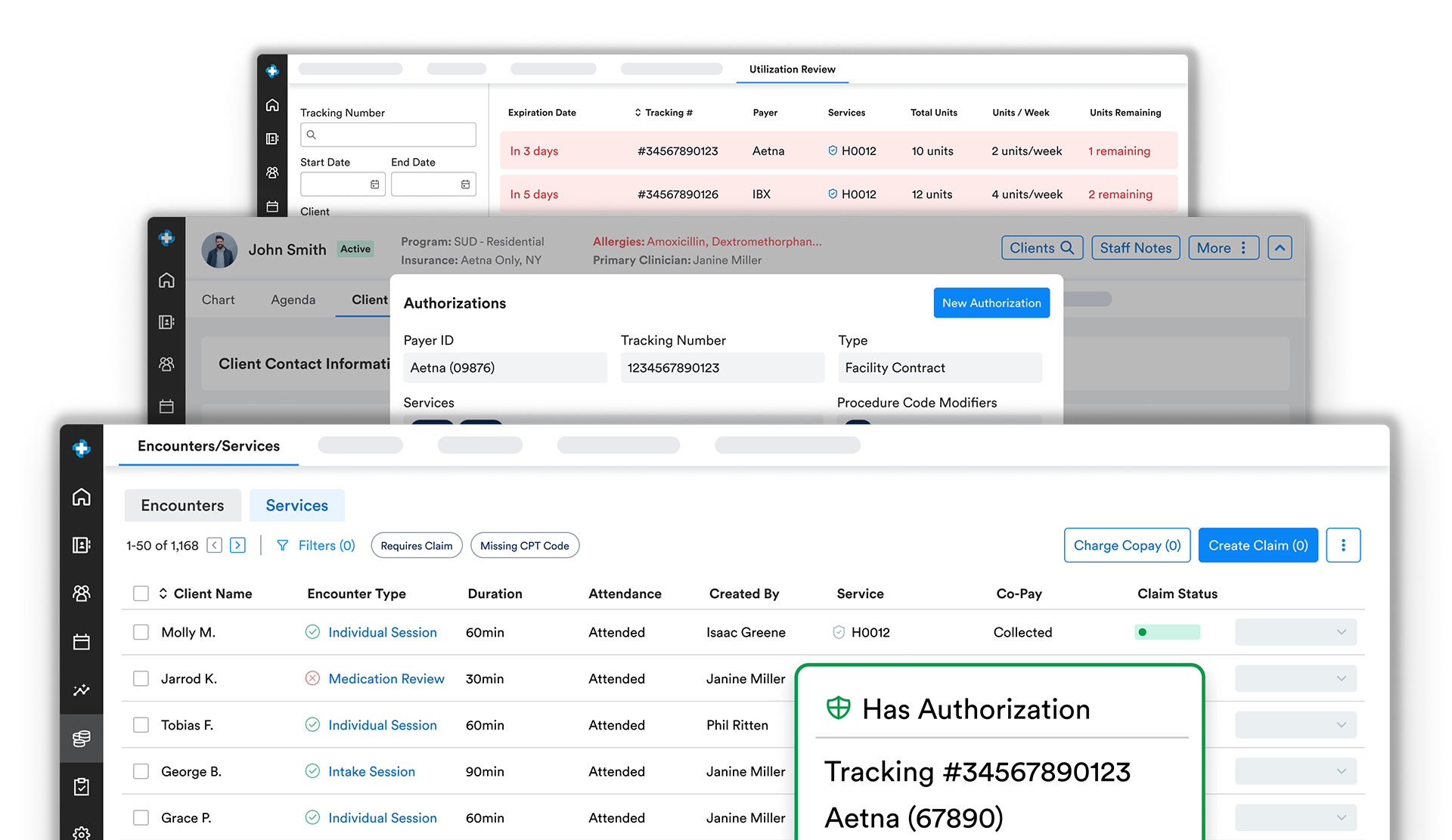
Ritten’s utilization review and authorization tools keep all your behavioral health authorizations in one place so you can prevent denials, stay ahead of expirations, and protect revenue.
How does Ritten manage behavioral health authorizations?
Authorizations shouldn’t live in email threads, PDFs, or staff memory. Ritten’s Utilization Review tools bring auth tracking into the same system where you schedule, document, and bill.
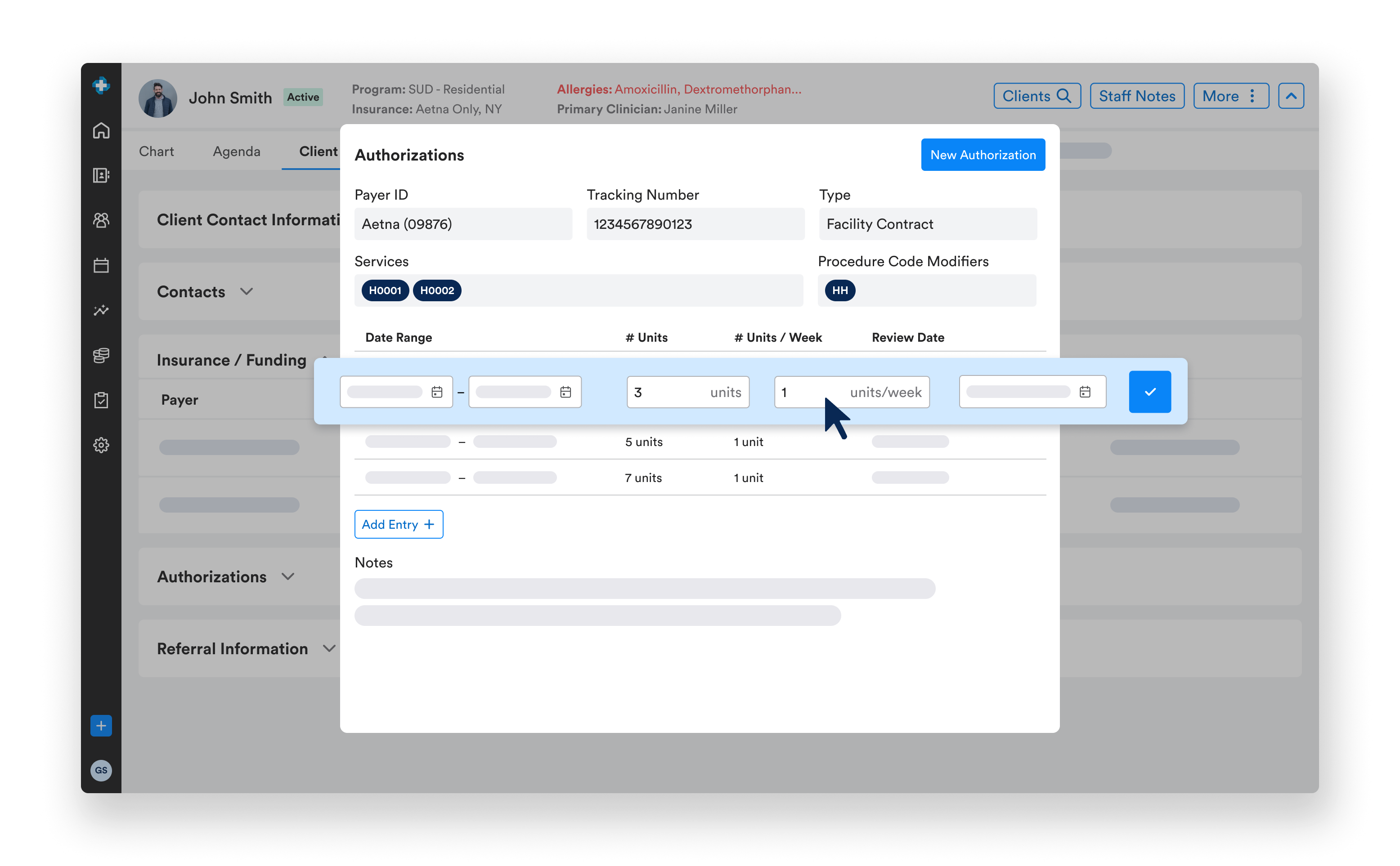
- Authorizations tied to payers and codes: Ritten tracks all authorizations. The appropriate auth automatically populates on claims with the correct payer and CPT code.
- Track expirations and remaining units: Built-in tracking for expiring and depleting authorizations let you know when it's time to request more sessions.
- Program-aware: Support for outpatient, IOP, PHP, residential, and SUD authorizations, including different limits and requirements by CPT code
Fewer authorization related denials, more predictable reimbursement
With authorizations visible in the same place as your encounters and claims, behavioral health teams can:
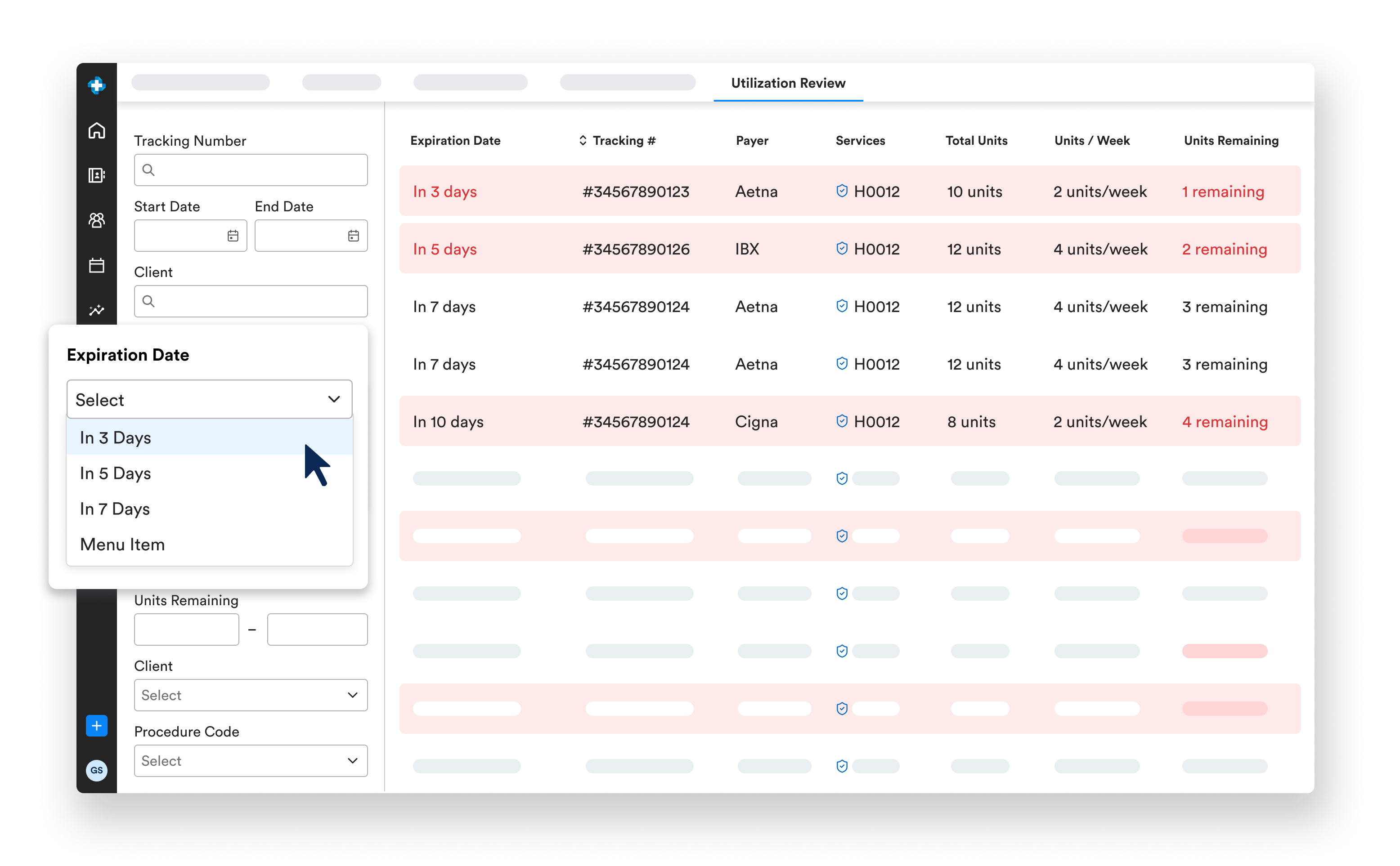
- See at a glance which clients are missing auths or are nearing limits.
- Plan ahead for utilization review calls and documentation.
- Avoid billing sessions that will be denied for lack of authorization.
- Keep clinicians focused on care while admin staff manage payer rules.
The result: fewer surprise denials, smoother utilization review conversations, and more predictable cash flow.
Authorizations aligned with documentation and payer rules
Linking authorizations to specific services and payers makes it easier to show:

- That billed services match approved services.
- That auth limits and renewal dates are being respected.
- That treatment decisions are documented and connected to payer authorizations.
This keeps you better prepared for audits and payer reviews while reducing the administrative burden on your clinical team.
Frequently Asked Questions
Still have questions about ourbehavioral health software? Email us at info@ritten.io
Yes. Ritten tracks remaining units and expiration dates and can surface which clients are approaching limits so your team can act before services are denied.
Yes. Most organizations move their UR spreadsheets into Ritten so everything—auths, sessions, and claims—is visible in one system.
Authorizations are linked to payers and CPT codes. When you bill, Ritten applies the appropriate auth details to the claim automatically.
Ritten fits into the way your program already bills and automatically generates the right claims. Whether encounters create claims directly, encounters bundle into per diem claims, or per diem claims are generated from program enrollment so your workflow never has to fit an encounter-based mold.
Ritten can track authorizations for outpatient therapy, psychiatry, IOP, PHP, residential treatment, and SUD programs across commercial and Medicaid payers.

