Automated Claims for Behavioral Health Billing
Claimification is Ritten’s one of a kind automated claims engine. It turns behavioral health encounters into clean CMS-1500 and UB-04 claims so your team can spend time resolving exceptions, not keying in codes
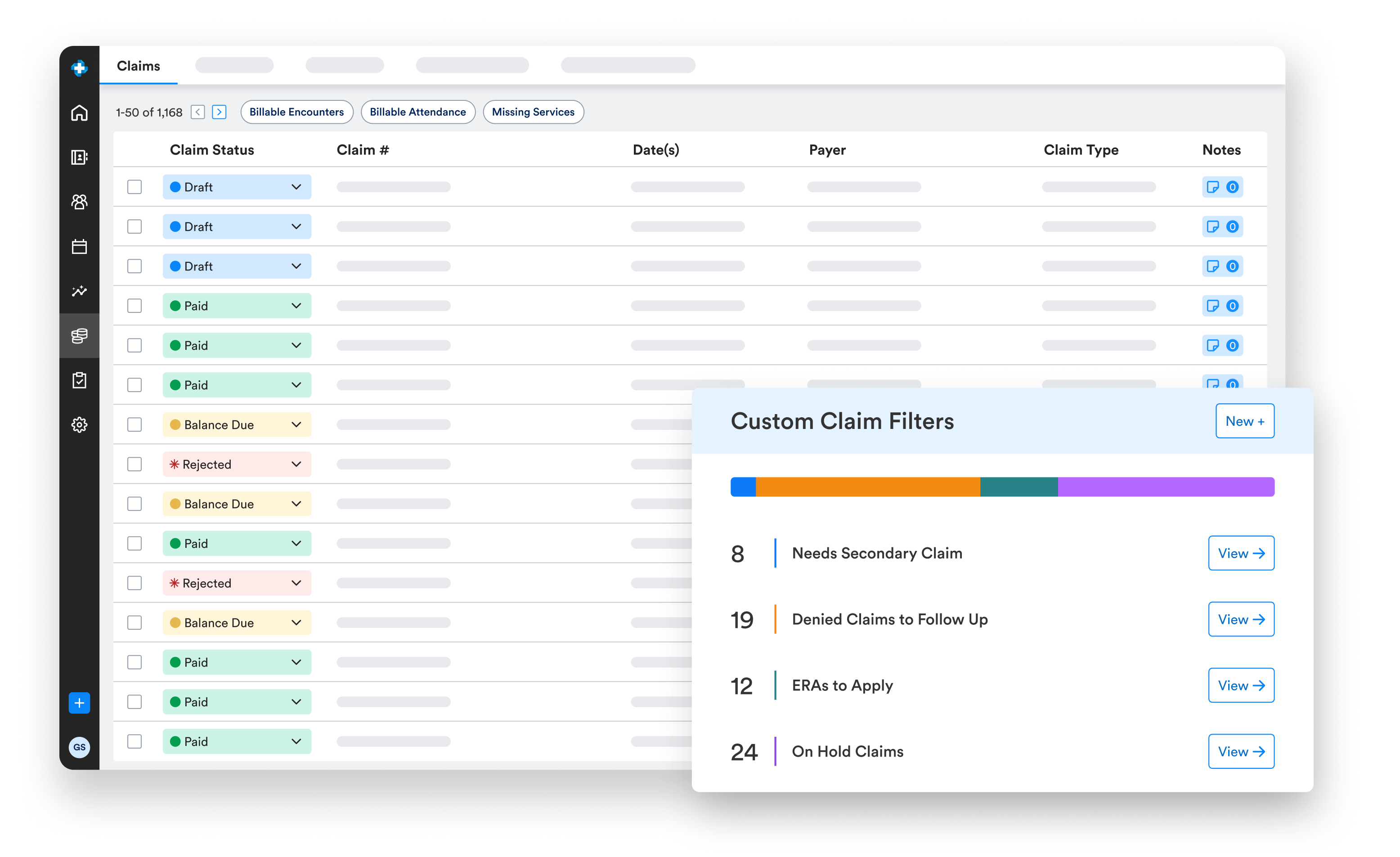
.png)
How does Ritten automate behavioral health claims?
With Claimification, each client encounter is automatically run through your billing rules. Codes, modifiers, and claim details are generated for you in the background no manual coding required and no separate billing platform needed.
Ritten automatically generates the right claims for inpatient/residential billing. Whether you bill by encounter, bundle encounters into per diem, or generate per diem claims from program enrollment, so you can keep your existing workflow while we handle the automation.
.png)
- Automated coding from Encounters: Every client encounter is automatically run through your billing rules and coded.
- Complete CMS-1500 & UB-04 generation: Automation generates entire CMS-1500 and UB-04 forms for behavioral health services, fully ready to be submitted.
- Works across payers and programs: Claimification supports private-pay, commercial payers, Medicare, and Medicaid, across outpatient, IOP, PHP, residential, and SUD programs.
- Supervisory billing support: Built-in handling for supervisory billing so claims meet payer requirements.
- Granular CPT logic for groups: Even in group services, clients can be billed differently depending on client, program, and payer.
You design the billing rules. Ritten runs them consistently.
Under the hood, Claimification is incredibly flexible. On the surface, it feels simple and predictable for your behavioral health billing team.
- Configure CPT codes, revenue codes, and modifiers by payer, program, and visit type.
- Map billing and rendering providers, facility/location details, and place-of-service logic.
- Manage fee schedules and service bundling without losing the clinical trail.
- Automatically match claims to ERAs and post payments, adjustments, and patient responsibility.
From all-day work to "done in an hour"
Before Ritten, many behavioral health billers documented in one system, billed out of another, and tracked payments in spreadsheets and payer portals. Claims might show as “accepted,” but not actually processed, forcing endless phone calls and portal logins.
.png)
With Ritten and Claimification:
- Claims are built and sent from one system based on your rules.
- Denials post back to the claim with the specific denial reason.
- Payments and adjustments auto-post from ERAs; billers focus on true exceptions instead of data entry.
Frequently Asked Questions
Still have questions about ourbehavioral health software? Email us at info@ritten.io
Yes. You can configure codes, modifiers, provider mappings, and fee schedules by payer, program, and level of care.
Yes. Claimification supports detailed Medicaid rules, including state-specific codes, modifiers, and program requirements.
Ritten supports capturing authorization and payer requirements and can connect encounter and documentation workflows to authorization rules. This is especially important in higher levels of care where approved dates, units, and medical necessity documentation must align to avoid denials.
Ritten fits into the way your program already bills and automatically generates the right claims. Whether encounters create claims directly, encounters bundle into per diem claims, or per diem claims are generated from program enrollment so your workflow never has to fit an encounter-based mold.
Claims that fail a rule or receive a denial are flagged for review, while the rest flow through automatically to keep your team focused on the highest-value work.
Claimification is Ritten’s automated claims engine that converts behavioral health encounters into CMS-1500 and UB-04 claims using your configured billing rules.

