Client payments and copays made managable
Ritten helps behavioral health and mental health organizations collect copays, handle private-pay, and manage client balances directly in the same system where you document and bill.

How does Ritten handle behavioral health client payments?
Ritten makes it easy to take payments at any point in your workflow and keep every dollar tied back to the right client, claim, and service.
- Flexible copay collection: Collect copays at any point in your workflow; up front on the day of service or later in the revenue cycle. It all syncs back to the client's chart.
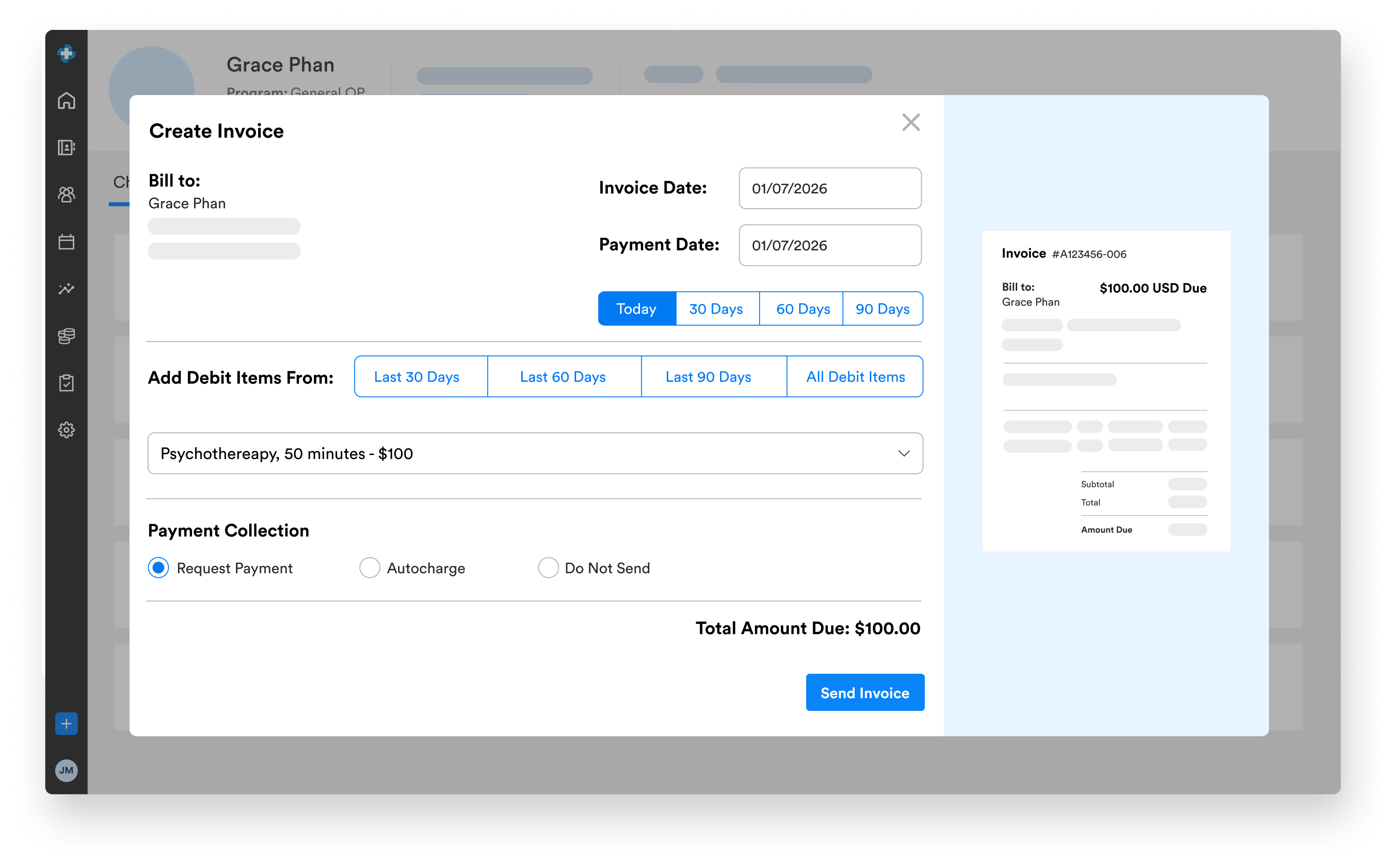
- Automated charging & invoicing: Highly automated client-charging workflows can auto-charge copays and auto-send invoices, reducing manual follow-up.
- Full private-pay support: Handle fully private-pay behavioral health clients with the same smooth workflows and visibility.
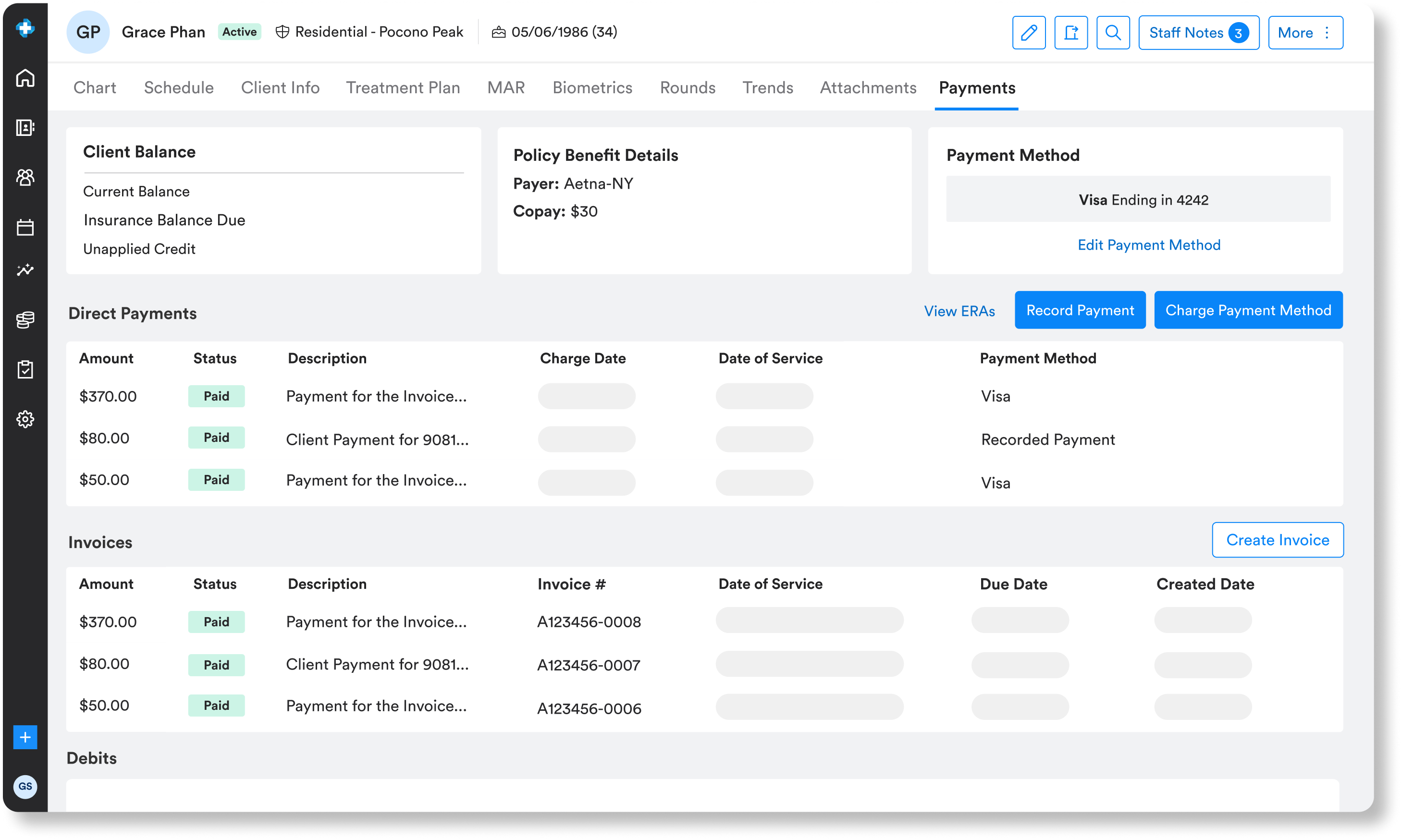
- Unified client balance view: Manage a client's payments, insurance balance, and unapplied credits from one place: their chart.
- Modern payment methods: Take credit cards and ACH payments directly in Ritten, and log payments mad outside of Ritten (like cash or chek).
Designed for front-desk staff, billers, and leadership
Client payments in Ritten work for everyone who touches the revenue cycle.
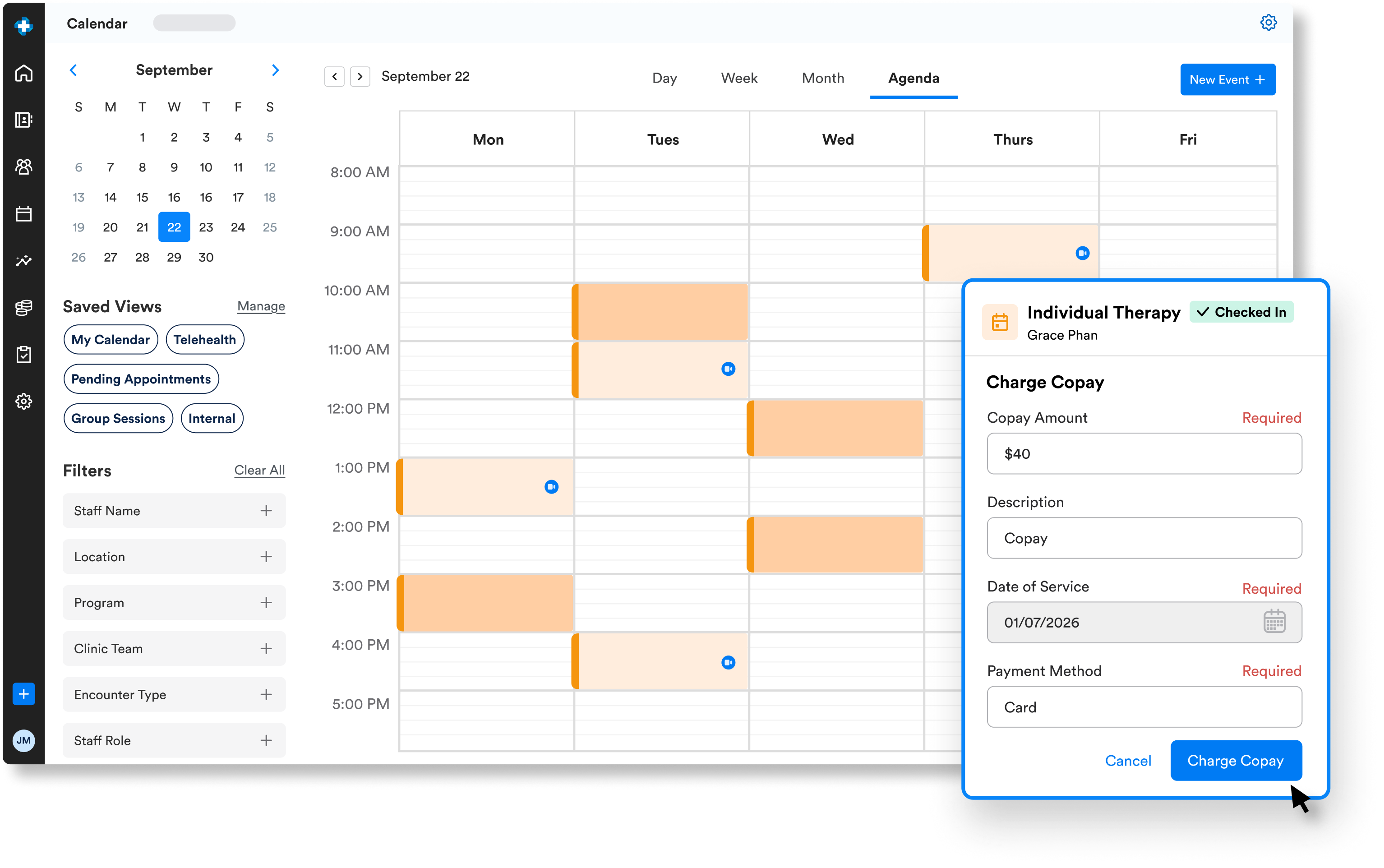
- Charge inside your workflow: Front-desk staff can charge from the calendar or client chart; billers can charge at any point in the pre- to post-claim workflow.
- In-app payments: Accept and record payments without bouncing between systems or third-party portals.
- Track cash & checks: Keep non-electronic payments in sync with the rest of your billing and reporting.
- Auto-generated invoices & superbills: Generate invoices and superbills in a couple of clicks so clients can seek reimbursement when needed.
Clear, accurate statements clients can understand
Because Ritten ties together claims, ERAs, and client payments, your team can send statements that:
- Reflect up-to-date balances.
- Clearly distinguish insurance responsibility vs. client responsibility.
- Reduce confusion and back-and-forth with clients.
- Improve on-time payments without aggressive collections tactics.
Frequently Asked Questions
Still have questions about ourbehavioral health software? Email us at info@ritten.io
Yes. You can set up workflows to automatically charge client copays once claims are processed and payer responsibility is clear.
Yes. Ritten provides a unified view of insurance balances, client responsibility, and unapplied credits in each client’s chart.
Ritten can support recurring payments and scheduled charges as part of your workflow; our team can help configure this based on your policies.
Payments are linked to specific services and claims, so your A/R and client balances stay accurate and audit-ready.
Ritten fits into the way your program already bills and automatically generates the right claims. Whether encounters create claims directly, encounters bundle into per diem claims, or per diem claims are generated from program enrollment so your workflow never has to fit an encounter-based mold.

